Foot and Ankle
Ankle Sprain/ Instability
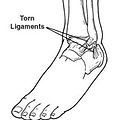
An ankle sprain is an injury to one or more ligaments in the ankle, usually on the outside of the ankle. Ligaments provide stability by limiting side-to-side movement. The severity of an ankle sprain depends on whether the ligament is stretched, partially torn, or completely torn, as well as on the number of ligaments involved.
Causes
Sprained ankles often result from a fall or a sudden twist. Symptoms Symptoms may vary in intensity, depending on the severity of the sprain.
Symptoms
May include: Pain or soreness Swelling Difficulty walking Stiffness
Diagnosis
A thorough history and examination is performed. X-rays are often ordered to determine the severity.
Treatment
Early treatment includes rest, ice, compression, and elevation. Physical therapy is initiated as soon as possible to promote healing and increase range of motion. Bracing helps control swelling, limit excessive movement and stabilize the ankle. Medications to reduce swelling and provide pain relief may be recommended.
What is Chronic Ankle Instability?
Chronic ankle instability is a condition characterized by a recurring “giving way” of the outer (lateral) side of the ankle. This condition of develops after repeated ankle sprains.
Symptoms
People often complain of a repeated turning of the ankle, especially on uneven surfaces or when participating in sports. The ankle feels unsteady and there is persistent pain or tenderness.
Diagnosis
A thorough examination of your ankle is performed to check for tender areas, swelling, and instability. X-rays and MRI may be helpful in further evaluation.
Treatment
Treatment is based on the results of the examination and tests, as well as on activity level. Non-surgical treatment may include: Physical Therapy, bracing, and medication.
In some cases, your doctor will recommend surgery based on the degree of instability or lack of response to non-surgical care. Surgery usually involves repair or reconstruction of the damaged ligament(s). Occasionally, a neighboring tendon is used to reinforce the repair. The length of your recovery will vary, depending on the procedure performed. Physical therapy is often required to regain full use of the ankle.


Dr. Bevilacqua has written on the subject of ankle instability. Click the link below to read a case written by Dr. Bevilacqua. The article highlights a surgical procedure used for the treatment of ankle instability.


Ankle Arthritis (Ankle Fusion and Total Ankle Replacement)
What is a Ankle Arthritis?
The ankle joint is composed of the bottom of the tibia and the top of the talus, which is completely covered with cartilage to allow for smooth motion. The breakdown and eventual loss of cartilage in the ankle can produce swelling and pain, and may eventually result in deformity, loss of joint motion, and decreased ability to walk.
Causes
Osteoarthritis of the ankle develops as a result of a structural abnormality in the foot or ankle or as a result of abnormal mechanics. A previous ankle injury, most often, an ankle fracture can result in arthritis.
Symptoms
Pain and swelling Difficulty walking
Diagnosis
The affected ankle will be evaluated and x-rays and other imaging studies may be ordered.
Treatment
Early treatment may include medications, orthotics/bracing, steroid injections and physical therapy. In situations when the pain has progressed or failed non-surgical care, surgery may be considered. In severe cases, an ankle fusion or ankle replacement surgery may be recommended. Dr. Bevilacqua will consider a number of factors when selecting the procedure that is right for you.
Ankle Fusion

Ankle and subtalar joint Fusion


Ankle Fractures
What is a Ankle fracture?
A fracture is a partial or complete break in a bone. Fractures in the ankle can range from the less serious avulsion injuries to severe breaks in the tibia and fibula, or both. Ankle fractures are common injuries that are most often caused by the ankle rolling inward or outward.
Symptoms
Symptoms include pain at the fracture site and an inability to walk (however, it is possible to walk on less severe breaks), significant swelling and bruising, and at times, blisters may occur over the fracture site.
Diagnosis
The affected limb will be evaluated and x-rays and other imaging studies may be ordered (CTscan or MRI).
Treatment
Treatment depends on the type and severity of the fracture. Early treatment includes rest, ice, compression, and elevation. Additional treatments include immobilization in a cast or splint.
For some ankle fractures, surgery is needed to repair the fracture and realign the ankle joint. The length of your recovery will vary, depending on the procedure performed. Physical therapy is often required to regain full use of the ankle.


Above are radiographic examples of ankle fractures treated surgical to realign ankle joint

Above is a radiographic example of ankle fracture treated in a "high risk" patient treated with a minimally invasive approach.

Adult Acquired Flatfoot (Posterior Tibial Tendon Dysfunction (PTTD))
What is PTTD?
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch.
PTTD is often called “adult acquired flatfoot” because it is the most common type of flatfoot developed during adulthood. PTTD is usually progressive, which means it will keep getting worse, especially if it isn’t treated early.
Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Treatment
Early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. Early treatment may include immobilization, physical therapy, medications, orthotic devices and/or bracing.
In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Surgery often includes repairing the posterior tibial tendon, tendon transfers and realignment osteotomies.


The radiograph on the left is from an adult patient with a severe painful flatfoot. He had undergone a previous surgery at another institution which failed to relieve his symptoms. After an extensive conservative approach, Dr. Bevilacqua performed a revisional reconstructive surgery to restore stability to his foot and alleviate his symptoms.

Charcot Foot Reconstruction
What Is Charcot Foot?
Charcot foot is a condition causing bone and joint destruction in the foot leading to severe foot/ankle deformity. It may occur in people who have nerve damage (neuropathy). The most common cause of nerve damage is from diabetes.
Often there is a delay in diagnosis and with continued walking the foot continues to deform and changes shape. Charcot foot is a very serious condition that can lead to severe deformity, disability, and even amputation.
Causes
Charcot foot develops as a result of neuropathy, which decreases sensation and the ability to feel temperature, pain, or trauma. People with neuropathy (especially those who have had it for a long time) are at risk for developing Charcot foot.
Symptoms
The symptoms of Charcot foot may include: Warmth to the touch (the affected foot feels warmer than the other). Redness and swelling in the area.
Diagnosis
Early diagnosis of Charcot foot is extremely important for successful treatment. Clinical examination, X-rays and other imaging studies and tests may be ordered. Once treatment begins, x-rays are taken periodically to aid in evaluating the status of the condition.
Treatment
Non-surgical treatment for Charcot foot consists of Immobilization and offloading. Complete non-weightbearing is necessary to keep the foot from further collapsing. It may take the bones several months to heal, although it can take considerably longer in some patients. Shoes with special inserts or custom shoes and bracing may be used after the bones have healed and help prevent recurrence of Charcot foot, development of ulcers, and possibly amputation.
When is Surgery Needed?
Charcot Foot is a disabling condition and is so severe that surgery, and occasionally amputation, may become necessary. Reconstructive surgery is performed to obtain a functional, plantigrade foot.
Come see us immediately if you notice signs of Charcot foot.

Here is a picture of someone that underwent Charcot Foot reconstruction with the use of external fixation

Here is a picture of someone that underwent Charcot Foot reconstruction with the use of internal fixation

Here is a clinical picture of someone that underwent extensive Charcot ankle reconstruction with the use of external fixation to correct deformity and realign the foot under the leg.
Dr. Bevilacqua has written extensively on the subject of Charcot foot and ankle. Click the images of the titles below to read some of the articles written by Dr. Bevilacqua.

Bunion (Hallux Valgus)
A bunion is often described as a bump on the side of the big toe. But a bunion actually reflects changes in the bony framework of the front part of the foot. Rather than point straight ahead, the big toe leans toward the neighboring toe and gradually changes the angle of the bones which produces the characteristic bump. Bunions are a progressive disorder and symptoms usually appear at the later stages.
Causes
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to develop a bunion.
Symptoms
May include: pain or soreness, inflammation, a burning sensation and possible numbness.
Diagnosis
Diagnosis begins with a careful history and physical examination by your doctor. Bunions are readily apparent, however x-rays will allow your doctor to measure several important angles to help determine the appropriate procedure.
Treatment
Early treatment includes: changes in shoe- wear, padding, activity modification, medications, icing, injection therapy or orthotic devices. If all conservative measures fail to control the symptoms, then surgery may be suggested.
A variety of surgical procedures are available and they are designed to remove the “bump”, correct the changes in the bony structure of the foot, and correct soft tissue changes that may have occurred. The goal of surgery is the reduction of pain.
Dr. Bevilacqua actively performs the LAPIPLASTY® procedure for bunion correction.
He also performs minimally invasive bunion (MIS) surgery when indicated. This newer technique for correcting bunions may result in faster recovery, less pain and swelling, smaller scars, and less reliance on narcotics.

Bunion (before surgery)

After surgery
In selecting the procedure, Dr. Bevilacqua will take into consideration the extent of your deformity based on x-ray findings, your age, your activity level, and other factors. The length of your recovery will vary, depending on the procedure performed. Dr. Bevilacqua performs minimally invasive bunion correction and he is well-versed in performing advanced procedures to precisely correct the metatarsal alignment to reduce recurrence of the deformity.

Achilles Tendinitis/ Rupture
What is the Achilles Tendon?
A tendon is a band of tissue that connects a muscle to a bone. The Achilles tendon runs down the back of the lower leg and connects the calf muscle to the heel bone. Also called the "heel cord," the Achilles tendon facilitates walking by helping to raise the heel off the ground.
What is an Achilles Tendon Rupture?
An Achilles tendon rupture is a complete or partial tear that occurs when the tendon is stretched beyond its capacity.
Causes
Forceful jumping or pivoting, or sudden accelerations of running, can overstretch the tendon and cause a tear. Achilles tendon ruptures are most often seen in "weekend warriors" – typically, middle-aged people participating in sports in their spare time. Less commonly, illness or medications, such as steroids or certain antibiotics, may weaken the tendon and contribute to rupture.
Symptoms
May include: Sudden pain (which feels like a kick or a stab) in the back of the ankle or calf. A popping or snapping sensation. Swelling and difficulty walking (especially upstairs or uphill) and difficulty rising up on the toes
Diagnosis
The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through a thorough clinical examination. In some cases (chronic or neglected ruptures), however, an MRI or other advanced imaging tests may be ordered.
Treatment
Treatment options for an Achilles tendon rupture include surgical and non-surgical approaches. The decision of whether to proceed with surgery or non-surgical treatment is based on the severity of the rupture and the patient’s health status and activity level.
Non-surgical treatment, which is generally associated with a higher rate of re-rupture, is selected for minor ruptures, less active patients, and those with medical conditions that prevent them from undergoing surgery. Non-surgical treatment involves use of a cast, walking boot, or brace to restrict motion and allow the torn tendon to heal.
Surgery offers important potential benefits. Besides decreasing the likelihood of re-rupturing the Achilles tendon, surgery often increases the patient’s push-off strength and improves muscle function and movement of the ankle. Various surgical techniques are available to repair the rupture. Dr. Bevilacqua will select the procedure best suited to the patient and offers a minimally invasive approach to repair the Achilles tendon rupture.
Following surgery, the foot and ankle are initially immobilized in a splint and then patients are transitioned to a walking boot. Physical therapy is an important component of the healing process. Physical therapy involves exercises that strengthen the muscles and improve the range of motion of the foot and ankle.
Acute Achilles tendonitis
Is an irritation or inflammation of the large tendon in the back of the lower calf that attaches to the back of the heel. In some, the thin tissue surrounding the tendon (paratenon) gets inflamed as a result of rapid acceleration and deceleration of the foot. The condition is often present in individuals who overpronate (roll their foot inwards).
Treatment
Treatment of acute inflammation begins with rest, physical therapy, anti-inflammatory medicine, and at times, immobilization. If these measures do not fix the problem, surgery may be required to remove the inflamed lining of the tendon.
Chronic Achilles Tendnosis
This chronic condition is associated with gradual degeneration of the tendon. The tendon and the leg is painful, and pushing off may be painful and weak. The Achilles tendon is visibly thickened and swollen.
Treatment
Treatment includes physical therapy, and may include immobilization of the leg in a walking boot. The treatment of this condition is difficult because there is limited potential for the tendon to heal due to the lack of good blood supply. Nonetheless, there are patients who can manage without surgery , even though the tendon remains abnormal, it may not be painful. If pain and weakness persist, surgery may be necessary to repair and reconstruct the tendon and occasionally, a neighboring tendon is used to reinforce the repair.
Chronic Achilles tendon rupture
Neglected Achilles tendon ruptures are disabling injuries and one must appreciate the increased complexity of the situation. Surgical management is recommended for active individuals.
Dr. Bevilacqua has written on the subject of chronic or neglected Achilles tendon rupture. Click the link below to read a case written by Dr. Bevilacqua. The article highlights a surgical procedure used for the treatment of a neglected Achilles tendon rupture.

This patient is 5 months after surgery performing a single leg heel lift after undergoing a minimally invasive Achilles tendon repair surgery after rupturing his Achilles while playing soccer.


Hallux Rigidus (Arthritic big toe)
What is Hallux Rigidus?
Hallux Rigidus is a form of osteoarthritis involving the big toe joint. It causes pain and stiffness in the joint, and with time it gets increasingly harder to bend the toe. “Hallux” refers to the big toe, while “rigidus” indicates that the toe is rigid and cannot move.
Causes
Common causes are faulty function (biomechanics) and structural abnormalities of the foot. This “wear and tear” type of arthritis generally is associated with overuse- especially among people engaged in activities or jobs that increase the stress on the big toe joint. Hallux rigidus can also result from an injury.
Symptoms
Pain and stiffness in the big toe joint Difficulty walking or with certain activities Swelling and inflammation around the joint Difficulty wearing shoes due to a bone spur.
Diagnosis
A thorough examination is performed to evaluate the range of motion of the joint and X-rays help assess the severity of the deformity.
Treatment
Early treatment may include medications, shoe modifications, orthotics, injections, and physical therapy. In some cases, surgery is the only way to eliminate or reduce the pain. In selecting the procedure, the extent of deformity, age, and activity level are taken into consideration. The length of your recovery will vary, depending on the procedure performed.
In cases with severe arthritis surgery is indicated. In this situation, a first metatarsal-phalangeal joint (MTPJ) fusion was performed. This procedure eliminates the pain and restores function to the foot.

Amputation Prevention (Limb Salvage)
The world’s population with diabetes will increase from 171 million to 366 million by 2025. In the U.S., there are an estimated 24 million people with diabetes. Up to 25% of those with diabetes will develop a foot ulcer in their lifetime. That translates to roughly 1-2% of the diabetic patients per year. Diabetes is the leading cause of non-traumatic lower limb amputations.
In 2009, 1,571 non-traumatic amputations were performed in New Jersey due to the effects of diabetes.
What is a foot ulcer?
Diabetic foot ulcers are sores or wounds on the feet that occur in people with diabetes. If a foot ulcer goes untreated and does not heal, it may become infected, which may lead to amputation. Therefore, appropriate assessment and treatment of a foot ulcer is very important to prevent amputation.
Causes
In people with diabetes, prolonged high blood sugar levels are linked with damage to the nerves in the feet. Nerve damage can cause loss of sensation, as well as deformities of the feet. This nerve problem is called peripheral neuropathy.
Foot deformities, such as a bunion or hammertoe, can cause areas of high pressure which can lead to skin breakdown.
People can hurt their feet by repetitive minor trauma (such as walking) or by a single event (stepping on an object or wearing ill fitting shoes). Because of peripheral neuropathy, they may not notice the injury, which can lead to a diabetic foot ulcer. This is a common – and serious – complication of diabetes and can lead to a loss of your foot, your leg, or your life.
Charcot foot
This is a complex foot deformity. It develops as a result of loss of sensation and an undetected broken bone that leads to destruction of the soft tissue of the foot. This disabling complication is so severe that surgery, and occasionally amputation, may become necessary.
Poor blood flow
Poor blood flow to the feet is also common in people with diabetes, and this slows the wound healing process and increase the risk of infection and amputation. Dr. Bevilacqua works directly with vascular surgeons and may recommend consultation.
What we can do?
There are many new surgical techniques available to save feet and legs, including joint reconstruction and wound healing technologies.
Corrective Diabetic Foot Surgery
Foot and/or ankle deformities may cause instability or cause areas of high pressure which can lead to an ulcer or inhibit ulcer healing. At times, a corrective foot surgery is necessary to remove the deformity to assist in wound healing and ultimately prevent amputation. In selecting the procedure, Dr. Bevilacqua will take many factors into consideration. The length of your recovery will vary, depending on the procedure performed. Dr. Bevilacqua has published extensively and has lectured nationally and internationally on the subject of diabetic foot surgery.
When Is Amputation Necessary?
Even with preventative care and prompt treatment of infection and complications, there are instances when partial foot amputation is necessary to remove infected tissue, save a limb, or even save a life.

This picture compares the pressure analysis pre and post surgery. The foot on the left has a severe deformity that has resulted in a wound on the bottom of the foot. The picture on the right shows the same foot after corrective surgery. The pressure has been reduced under the midfoot and this allowed the wound to heal.
Ankle Arthroscopy
What is Ankle Arthroscopy?
Foot and ankle arthroscopy is a minimally invasive surgical technique that is a valuable adjunct to the diagnosis and treatment of certain disorders of the foot and ankle. This technique provides a direct “eyeball” visualization inside the joint. The indications for this procedure continue to evolve.
Ankle arthroscopy is generally performed as an outpatient surgery under general anesthesia with or without a regional pain block. It may minimize other problems encountered with large incisions around the ankle such as pain, bleeding, wound breakdown, and infection. Patients may be able to begin rehabilitation sooner, rehabilitate more functionally, and return to high level activities such as sports.
Arthroscopy utilizes a small camera with magnifying lenses, fiberoptics, and a digital video monitors to allow the surgeon to directly visualize the inside of an ankle.
What conditions is Ankle Arthroscopy used to treat?
Synovitis
Synovitis is inflammation of the soft tissue lining of the ankle joint (synovium) that will often manifest as pain, swelling, and loss of motion. This can occur due to an acute trauma, inflammatory arthritis (i.e. rheumatoid arthritis), overuse, and degenerative joint disease (osteoarthritis). If nonsurgical treatment options fail to provide relief, ankle arthroscopy can be used to surgically remove inflamed synovium.
Ankle Impingement
Anterior Ankle Impingement (also referred to as “athlete’s ankle” or “footballer’s ankle”) and Anterolateral Ankle Impingement- These occur when bone and/or soft tissue of the anterior (the “front” of) ankle joint becomes inflamed due to repetitive stress or irritation. This will cause pain in the ankle joint, swelling, and can limit motion of the ankle, especially dorsiflexion (loss of the ability to bend your “toes towards your nose”). The diagnosis of anterior ankle impingement can be made by physical exam and identifying osteophytes, or “bone spurs,” on standard x-rays of the ankle. Sometimes a MRI is necessary if bone spurs are not present. If nonoperative measures fail to relieve symptoms of either of these conditions, ankle arthroscopy can be used to shave away redundant soft tissues and/or bone spurs to relieve the symptoms.
Posterior ankle impingement occurs when the bone and soft tissue of the ankle and hindfoot (the “back” of the ankle) becomes inflamed due to repetitive stress. This will cause pain in the ankle joint, swelling, and often times limited motion of the ankle, especially plantarflexion (loss of the ability to “press on the gas”). This overuse syndrome occurs most commonly in ballet dancers, but can also be seen in other athletes. Like anterior ankle impingement, it is usually associated with bone issues, in the posterior part of the ankle (the “back” of the ankle). It can also be associated with an accessory bone, which is not found in all patients that is referred to as an os trigonum. Bone spurs, inflamed soft soft tissue, and if present, the os trigonum, can then be removed arthroscopically.
Loose bodies
Articular cartilage and/or scar tissue following trauma to the ankle can become free floating in the joint and form what is referred to as a “loose body”. These loose bodies can cause problems such as clicking, catching, and frank locking that often lead to pain, swelling, and loss of motion. Ankle arthroscopy is a minimally invasive technique that can be used to find and remove the loose body.
Osteochondral defect of the talus (also referred to as osteochondritis dessicans, OCDs, osteochondral fractures)
These are injuries to the articular cartilage lining the joint that can be caused by both acute or chronic trauma. This includes acute ankle sprains and repetitive ankle injuries caused by chronic ankle instability. Symptoms may be vague, but often include deep aching pain, stiffness and swelling, and clicking and/or locking. The diagnosis is made with the combination of physical exam and diagnostic images (x-rays, MRI, and/or CT scan). The treatment will be based on the size and location of the OCD, associated symptoms, patient demographics, and activity demands of the patient. After the diagnosis is made, treatment options include microfracture, subchondral drilling, abrasion arthroplasty, fragment fixation, and bone grafting procedures.
The indications and conditions treated with ankle arthroscopy is expanding and new and exciting techniques continue to emerge.


Intra-operative picture showing the removal of synovitis with an arthroscopic shaver
Anterior lateral ankle impingement (left). After removing soft tissue with an arthroscopic shaver (right).


